Management
Biden administration to roll back the Betsy DeVos Title IX rules
New Education Department regulations would undo Trump administration changes to sexual discrimination policies at U.S. colleges and universities, now requiring the schools to have in place measures to offer support to students and employees alleging discrimination.
Pay & Benefits
OPM has new tools to fight improper health insurance enrollments
Watchdog agencies and Congress have previously chided the federal government’s HR agency for the lack of internal controls ensuring that family members of federal workers and retirees remain eligible for the federal workforce’s health insurance program.
Pay & Benefits
Justice Department outlines benefits rule for Havana syndrome victims
A new interim final rule details how the department would compensate employees and dependents with qualifying brain injuries from anomalous health incidents.
Tech
TSA looks to AI to enhance x-ray screenings of travelers’ luggage
The Transportation Security Administration is already using facial recognition to verify the identity of travelers but wants to improve its scanners to detect more prohibited items.
Sponsor Content
Modernizing public health care
Discover how Optum Serve helped leading federal agencies address systemic problems and improve community health and well-being efficiently, effectively and sustainably.
Workforce
Pekoske touts impact of pay increases at TSA budget hearing
Workforce attrition has halved since the implementation of a new pay system that mirrors the General Schedule, while employee morale has reached its highest ever, according to the annual Federal Employee Viewpoint Survey.
Pay & Benefits
Postponing retirement problems: Part 1
It’s important to know the difference between a postponed retirement and a deferred retirement.
Workforce
New bill would create federal grant program for digital upskilling
The proposed Digital Skills for Today’s Workforce Act would add digital skills training to grant programs that provide education and professional development services in an effort to boost the talent pipeline.
Sponsor Content
Navigating the AI revolution: Strategies for ethical implementation in federal civilian agencies
An industry expert offers an insightful demystification of AI, delving into core principles and best practices the company infuses into service, as well as advice for an ever-changing future.
Oversight
Senate rejects impeachment articles against DHS Secretary Mayorkas
In a 51-49 vote along party lines, Senate Democrats dismissed impeachment charges Wednesday against Homeland Security Secretary Alejandro Mayorkas for not meeting the threshold of high crimes and misdemeanors.
FEATURED INSIGHTS
Oversight
When -- and how often -- are SBA staffers going into the office? A senator wants the agency's IG to find out
Sen. Joni Ernst, R-Iowa, continued her criticism of federal agencies’ use of telework, calling for the Small Business Administration’s inspector general to investigate its office utilization rates after its administrator disputed the GAO’s findings.
Management
Biden’s FLRA nominees move closer to Senate confirmation
Senators appeared poised Wednesday to advance the nominations of aspiring leaders in labor-relations.
Tech
NIST adds 5 new members to its AI Safety Institute
The new members will focus on AI objectives related to national security, standards development and more.
TSP TICKER
FUND
G
F
C
S
I
APR 19 CLOSE
$18.1925
$18.6420
$77.7675
$76.0678
$40.5384
DAILY CHANGE
0.0021
0.0235
-0.6835
-0.0474
-0.1313
THIS MONTH (%)
0.22
-2.30
-5.40
-7.72
-4.78
FUND
L 2060
L 2050
L 2040
L 2030
L INCOME
APR 19 CLOSE
$15.4916
$31.2104
$52.1654
$46.0536
$25.2480
DAILY CHANGE
-0.0876
-0.1427
-0.2087
-0.1539
-0.0336
THIS MONTH (%)
-5.46
-4.65
-4.08
-3.39
-1.41
FUND
APR 19
CLOSE
CLOSE
DAILY
CHANGE
CHANGE
THIS
MONTH
MONTH
G
$18.1925
0.0021
0.22
F
$18.6420
0.0235
-2.30
C
$77.7675
-0.6835
-5.40
S
$76.0678
-0.0474
-7.72
I
$40.5384
-0.1313
-4.78
L 2050
$31.2104
-0.1427
-4.65
L 2040
$52.1654
-0.2087
-4.08
L 2030
$46.0536
-0.1539
-3.39
L 2020
$None
None
L INCOME
$25.2480
-0.0336
-1.41
Pay & Benefits
Estate planning for federal employees: Maximize benefits and minimize taxes
Make sure to review and update your estate plan regularly to reflect changes in your financial situation and personal circumstances.
Tech
Feds move to make gov websites more accessible to people with disabilities
It’s the first time the federal government has ever issued rules clarifying how the more than 30-year-old Americans with Disabilities Act applies online. But the new rules come with a hefty price tag for state and local governments.
Management
Texas Republicans urge Senate Democrats to give the DHS secretary a full impeachment trial
The House voted to impeach Alejandro Mayorkas on Feb. 13 over charges of refusing to enforce the law and “breach of public trust.”
Tech
100,000 have used IRS Direct File to submit their tax returns
The agency has not yet determined whether the pilot program for the tool will be extended into a permanent offering.
Management
OPM Director will leave the Biden administration
Kiran Ahuja oversaw efforts to transform the federal government’s HR agency into a government-wide leader on human capital policy, issuing new policies governing interns, telework and civil service protections.
Pay & Benefits
VA is trimming its PACT Act claims backlog, but enrollees may be on the ‘low side’
Veterans Affairs Secretary Denis McDonough says that the department is quickly processing new claims made by veterans exposed to toxic substances during their military service, thanks, in part, to robust hiring, but warns that those claims may not have hit their peak yet.
Pay & Benefits
Bill wants to solve the coverage gap for National Guard and reservists by extending VA eligibility
Legislation from Rep. Joe Neguse, D-Colo., proposes to expand VA health care benefits to personnel in the reserve components when not on active duty to help ensure “force readiness.”
Workforce
Biden rescinds COVID-era executive orders, folding safer federal workforce task force
The Office of Personnel Management issued new guidance last week rescinding some forms of COVID-19-related administrative leave, but preserving four hours of paid leave for federal employees to get vaccine booster shots.
Management
Senate Republicans push for Mayorkas impeachment trial
Democrats say the charges are based on policy disputes rather than the “high crimes and misdemeanors” threshold of an impeachable offense.
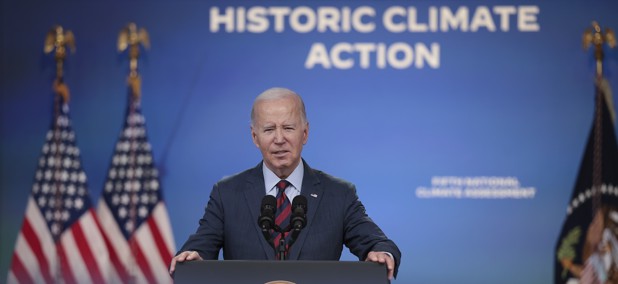
Management
Biden’s environmental justice scorecard offers more questions than answers
The White House's own environmental justice progress report gives little insight into the green benefits delivered to disadvantaged communities.
Oversight
HHS removed Login from its grantee payment system after funding theft
Hackers used data from a federal contracting hub to steal funding from seven grantee organizations in an HHS breach that occurred last year. Both HHS and GSA say that Login.gov was not compromised or connected to the theft.
Management